Quin Bradley’s diabetes diagnosis took her by surprise. “I had blurred vision and was having a hard time sleeping,” recalls the Kentucky business consultant. She had put on 30 to 40 pounds and then suddenly dropped the weight. “But I didn’t link any of those things to diabetes.” It was her mother who insisted she see her doctor. “The doctor did a blood test and called to tell me that my numbers were so high that they couldn’t get an accurate reading and that I should go to the emergency room,” says Bradley, 40. The diagnosis caught her completely off guard. Indeed, diabetes comes as a surprise to many. The Centers for Disease Control and Prevention says 4.9 million African-Americans ages 20 or older—almost 19 percent—have the disease, but only about one in four of us knows it.
A diabetes diagnosis can be over- whelming for the person who receives it as well as for the people who love her. Fortunately, if you’re armed with good information and a solid action plan, you can still live well. Here are some tips to help you manage and control diabetes so that it doesn’t control you.
Get Smart
“Ninety-five percent of diabetes management is self-care,” says Michelle Gourdine, M.D., the author of Reclaiming Our Health: A Guide to African American Wellness. A doctor can diagnose and advise but, day- to-day, your care is up to you. Gourdine urges newly diagnosed patients to learn as much about the disease as possible.
Quiz your doctors, then do your research on how to make lifestyle changes that will keep you healthy. Gloria Cousar, 64, a Reston, Virginia–based urban plan- ner, not only read up on diabetes but also spent time at a health center to learn to incorporate diabetes self-care into her life. There she learned strategies to reduce stress, monitor her blood sugar, prepare diabetes-friendly foods and exercise.
Take Your Medicine
“If type 2 diabetes is diagnosed early enough, oral medications are usually the first treatment option,” says Gourdine. The trick is remembering to take them. A phone app like MedCoach Medication Reminder tells you which medications to take when.
If your glucose levels can’t be controlled with oral medications, you may be prescribed injectable insulin or an insulin pen either alone or in combination with pills. You have to time your injections so insulin starts to work at roughly the same moment glucose from your meal enters your bloodstream, according to American Diabetes Association guidelines. That means planning your mealtimes, then timing your injection accordingly.
Cousar decided to move from an injectable to an insulin pump. The device can be programmed to release insulin in doses throughout the day and at meal-times. If you and your doctor decide this is the best route for you, you’ll have a minor surgical procedure to insert the catheter under your skin, and get training on how to use the device. After that, you’ll wear the pump almost all the time—taking some of the worry out of remembering insulin doses.
Track your Numbers
Be vigilant about monitoring your blood sugar during the day with a glucometer, a tool that takes a small sample of blood and measures your glucose levels. An app like Glooko, Glucose Buddy or OnTrack Diabetes can help you remember when to test—and then record your numbers and insulin doses. Some apps also allow you to track your weight, blood pressure and activity level, as well as share that information with your health care provider.
Get Moving
Daily exercise is essential, says Valerie W. Hogue, associate dean at Notre Dame of Maryland University School of Pharmacy. Regular exercise can make your body more sensitive to insulin, according to experts. And during exercise, your cells remove glucose from the blood so your sugar is lower.
“Try to make it a habit every day,” says Hogue, who is also a certified diabetes educator. “I recommend 150 minutes of some kind of moderate physical activity per week.” That’s just a little more than 20 minutes a day. Set your alarm clock a half hour earlier and get up for a brisk walk or a mini workout at home. Or sign up for a fun exercise class that you won’t want to miss. “I have a pet that I have to walk, and that helps me get exercise,” Cousar says.
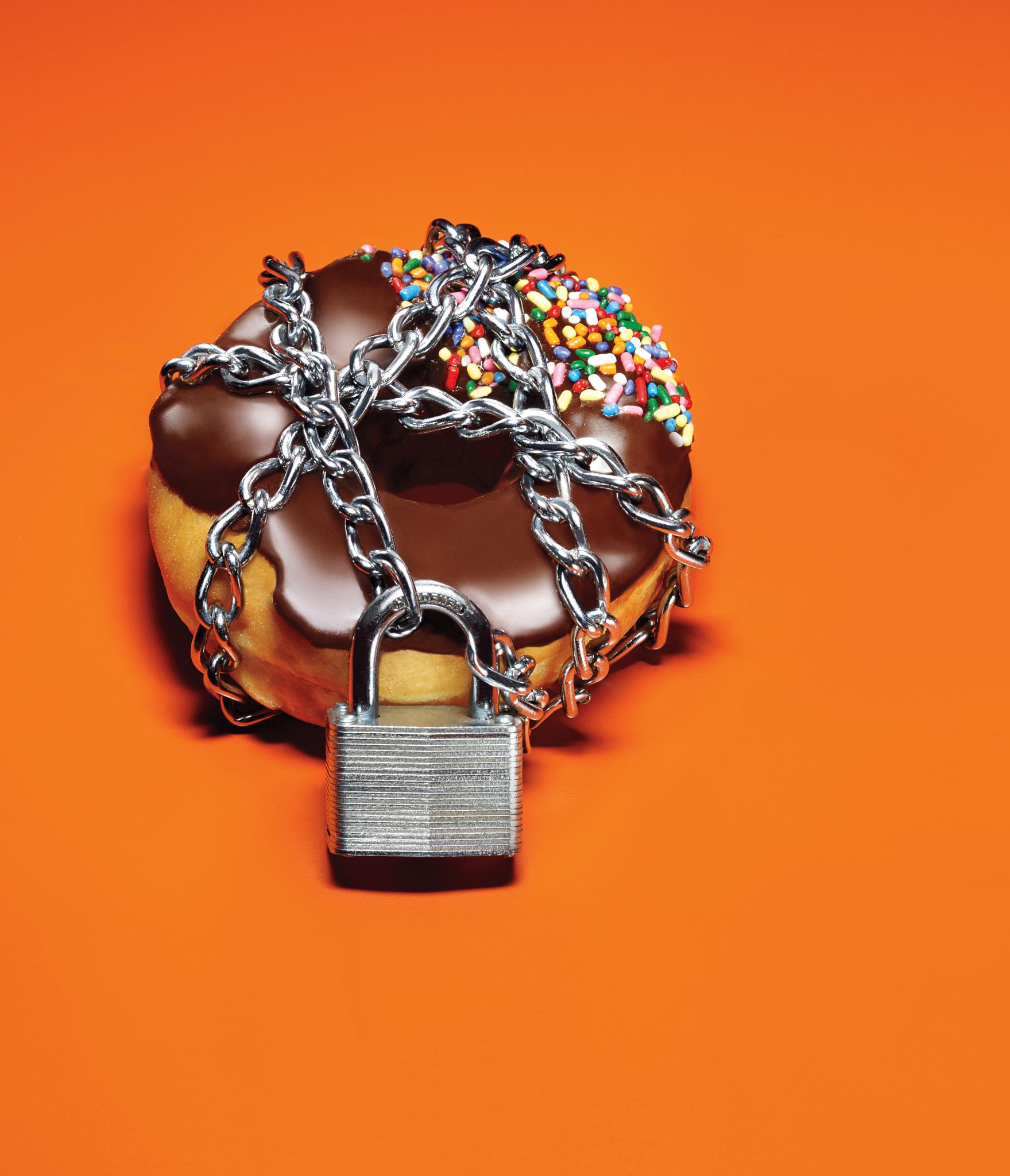
Detail Your Diet
Managing your blood sugar is closely linked to your diet. Plan meals carefully and be mindful of portion sizes, Hogue says. Experts recommend lean proteins, low-carb vegetables and whole grains. “And stay away from processed foods that are high in hidden sugars and salt,” warns Gourdine.
But how can you avoid the “bad stuff” in your pantry? Cousar says she cleaned out the kitchen to make room for diabetes-friendly foods. She mostly uses no-cal/low-carb sweeteners instead of sugar; nuts and seeds now sub for chips, and she also stocks up on fruits, vegetables and fiber-rich foods.
The Fooducate app and Web site (fooducate.com) can help you be aware of the ingredients in the food you are eating, including those high in sugar.
Imbibe Intelligently
Bradley switched from sodas and coffee to water. No-cal flavored water or sparkling water can add a little sweetness to your water regimen. For a treat, “I make smoothies with vegetables and fruits,” she says. She also limits alcoholic beverages, which are high in sugar.
Check Your Stress
Stress hormones can directly alter your blood glucose levels, experts say. And often stress may make you want to drink more alcohol, eat fatty comfort food and veg out instead of exercise—none of which is good for diabetics. While a person with diabetes can’t always control the stress she encounters, it is important to find ways to manage your reaction to it.
First step: Aim for seven to eight hours of sleep a night. “Being chronically sleep-deprived can keep you stressed,” says Gourdine. If you’re rested, you are likely to have a more clearheaded response. What if you’re too stressed to sleep? Exercise, meditation and deep breathing can all help you relax.
Don’t Do it Alone
Taking care of yourself isn’t always easy, but Hogue says it’s important to get support. “Don’t just count on your doctor, but also reach out to your family and friends in your journey,” she says.
This article was originally published in the November issue of ESSENCE magazine, on newsstands now.



