In early March, a little over a week before COVID-19 became a global pandemic, ESSENCE published a story about the perceived impact of the coronavirus on African American communities. At the time, the American public was only slightly aware of the virus’s severity—and many African Americans were still doubtful that Black people could, in fact, get it.
Responses to the article, which mainly advocated for health insurance and paid sick leave, ranged from concerned to optimistic, with the majority landing on unbothered. “This is bullshit, and I don’t believe none of this,” one Facebook user wrote. “Wash your damn hands and you will turn out just fine.” Another noted, “Not a single black person has gotten this. One in Africa, but he recovered.” “The devil is a lie,” a third said. “How bout we drinking ginger ale now.” And a popular response: “Question—All these celebrities who have constant interaction with the public, almost on a daily basis, not one declared ill, no comments from any of them regarding the issue. All news and government gossip.”
In the words of avid Twitter users, those comments did not age well. But they do convey the sentiments of a swath of skeptical African Americans just three weeks ago. Time has proven that Black people can get it and washing our hands won’t change that; nor will ginger ale, Vicks or Robitussin, for that matter. Confirmed deaths of Black men and women across the nation have also proven that the illness and its implications are not “government gossip” but a very real thing.
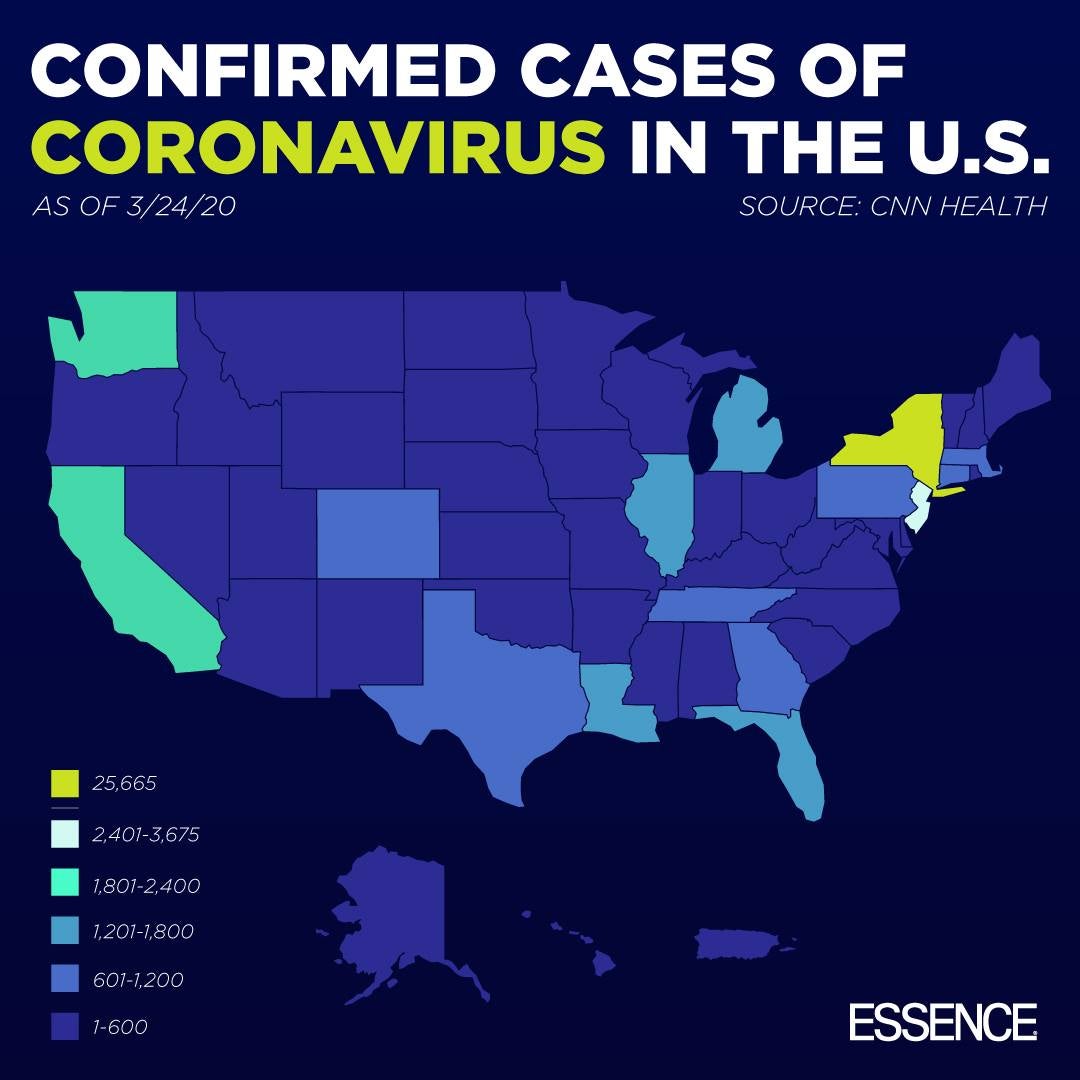
To date, the novel coronavirus has killed more than 1,000 people in the United States and significantly more around the globe. It’s left us self-quarantining, sheltering in place, and washing and disinfecting our surroundings ad nauseam. But even with following the recommended steps to a tee, there is no guarantee that many of us won’t get it.
Dr. Maggie Cadet, a rheumatologist in New York City, is regularly dealing with what the uncertainty of catching “the Rona” may mean for her patients. As a medical professional who treats those who are immunocompromised, she understands even more so the angst that the outbreak has caused. Cadet spoke with ESSENCE last week to share her expert advice. More specifically, what we should do if and when the coronavirus hits our home?
Know The Symptoms
“At this time, we don’t know this virus, and it’s really uncharted territory,” Cadet explained. “We have to treat it like it’s a war. We have to really do our part and be knowledgeable of the symptoms.”
Though many people have compared the pandemic-size illness to the seasonal flu, Cadet warns that there are distinct differences one should be aware of—in particular, shortness of breath. While headaches, sore throat, aches and pains, or even a runny nose could be experienced with both, the disease’s tendency to attack the lungs makes severe breathing complications a tell-tale sign. Others have reported a sudden loss of taste or smell. And Dr. Arabia Mollette, an NYC-based emergency physician, said to be on the lookout for diarrhea and conjunctivitis (inflammation in or around the eye). Both symptoms have been reported in a number of cases she’s treated.

Know Your Next Steps
If someone meet CDC criteria for the virus, Mollette directs them to call their primary care physician, urgent care center or nearest emergency department and inform the physician or allied healthcare worker of their symptoms. Cadet says even when you call 911 or an ambulance, you have to be transparent about what you are experiencing. “Health care practitioners also have to protect themselves and wear protective equipment,” the part-time medical blogger explains. “So that may include a PPE mask, gloves, gowns, and eye-protective wear.”
Molette shares that upon arrival, a mask is also immediately placed on the patient before they are escorted to a special room for isolation. The doctor will then swab the back of the throat and deep into the nose for aerosolized droplets. The swabs are sent to a state-run testing lab. If symptoms are less severe, drive-thru testing is another tool that helps improve surveillance of the virus and reduces the pressure on emergency rooms. Cadet points out that it also reduces the spread.
“Right now, if patients are having fever or other mild symptoms, like runny nose, a little bit of a cough or a feeling of malaise, they’re advised to call their doctors and ask if they should come in,” says Cadet. “If they are exhibiting symptoms and they can be seen on-screen (via a virtual doc), a doctor would know whether the patient needs to go to the ER or can stay at home or do urgent care. Using technology really is essential during this time.”

In every instance, whether it’s an ER visit, a drive-thru medic, or a digital appointment with a doc, potential COVID-19 sufferers are encouraged to self-quarantine or isolate as they await their results. A doctor will ultimately decide if acute respiratory symptoms will require hospitalization, a ventilator or other work-ups. Severe cases aside, Cadet simplified the recovery process by saying, “There’s not much to do, honestly, except for rest, supportive care and fluids.”
Know Your Risks And The Risk You Pose To Others
Though the illness has been known to wreak havoc on the bodies of those old and young, fit or unfit, generally healthy and otherwise, Dr. Cadet warns that patients who suffer from rheumatoid arthritis, lupus or other autoimmune diseases, like scleroderma, are at a higher risk. Regular medications can also lead to increased risk of infection and further suppression of the immune system. She cautions those people to take those factors into consideration when assessing how they feel.
For those who doubted or continue to doubt the severity of the disease, Cadet asks that they make themselves aware of the breadth of the coronavirus. There’s no known ethnic predisposition at the moment, but African Americans are more at risk for diseases that would cause complications with the illness. These include heart disease and diabetes, as well as hypertension.

To make sure that we’re protecting ourselves and others, the NYU Langone doctor puts forth that everyone should consider themselves a potential carrier, despite the sign of obvious symptoms, and act accordingly. This means keeping a safe distance from immunocompromised individuals, elderly loved ones and those with underlying chronic conditions that could be further complicated by the sometimes-fatal disease.
Know What Actions You Can Take Now
There’s no guarantee that a person won’t get COVID-19, no matter how much they do to try and prevent it. But Cadet recommends beefing up your vitamin C intake with things like spinach, broccoli and garlic. She also says to practice extreme cleanliness by leaving shoes at the door, disinfecting anything that’s been outside with Lysol spray, regularly wiping down surfaces and stripping off clothes that were exposed to the outside as you walk in your front door.

For the ladies going crazy without their hair and nail appointments, the self-proclaimed lover of beauty says it’s for the best. “Sometimes you’re getting a relaxer. A weave, a braid. It could be a three or four-hour process. And [the coronavirus] doesn’t even take 20 minutes to transmit.”
Most importantly she stresses that people should stay at home and quarantine themselves to try to prevent the spread. “I do believe if we’re not vigilant now for two to three or four weeks…we’re going to really have a hard time later.”

