
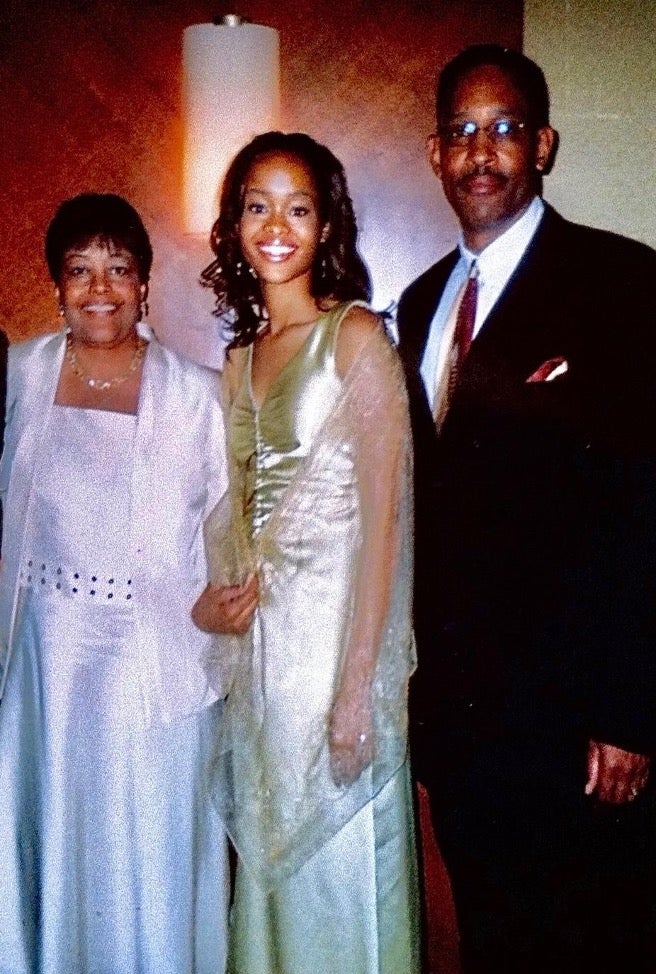
The year 2007 was heart-wrenching for Houston native Ashley Dedmon. Her mother, Lynn Armstrong, died of stage IV metastatic breast cancer at the age of 52.
She later discovered the disease was a silent killer no one in her family had discussed.
“Breast cancer aggressively attacked three generations of women and I didn’t know why they all succumbed to the disease,” she says. “I needed to get to work and ask questions to protect my health.”
Now is the ideal time to channel Dedmon’s energy for National Minority Health Month to do the work to learn the impact of genetics. Each exquisite strand of DNA shares a code about health risks that, if unknown or untreated, could have a significant effect on one’s life and lifespan.
Months after her mother’s death, Dedmon’s father was diagnosed with prostate cancer. He had surgery to remove it and now lives cancer-free. Paralyzed by fear that she could be the next family member to be diagnosed with cancer, she put her faith in God and made an important decision to break a familial cycle.
“I underwent genetic testing, as recommended by my gynecologist, and at the age of 22, I found out I carry the BRCA2 gene mutation,” she says. “That means I am at high risk for breast and ovarian cancers and have an elevated risk for other cancers. I learned I inherited it from my mother.”
Dedmon had her first mammogram at the age of 22 and began seeing a high-risk oncologist to monitor her breast and ovarian health. The next decade of her life included annual screenings, marrying the love of her life, Cameron and giving birth to two healthy daughters, Ava and Callie.
“During that season of my life, I saw myself repeating the same patterns as my mom, by putting everyone and everything before my health,” she recalls. “But I knew better and was educated and armed with information to preserve my life.”

In December 2016, at the age of 31, she underwent a bilateral prophylactic mastectomy, or preventative double mastectomy. In layman’s terms, the removal of both breasts. The procedure has been shown to reduce the risk of breast cancer by at least 95 percent in women who have a mutation in the BRCA1 or BRCA2 gene and by up to 90 percent in women who have a strong family history of breast cancer according to the National Cancer Institute.
Altovise Ewing, PhD, LCGC, is a health equity strategist and genetic counselor who amplifies efforts around genetic testing for African-Americans. Ewing reports that across the genetics research continuum, people of color are underrepresented at the participant, clinician and investigator levels.
“Genetic counseling and testing are services that can help patients and families better understand their risk and management options for various conditions,” Ewing explains. “Because the Black population is disproportionately impacted and burdened by multiple diseases, genetics services may serve as one of the tools in the toolkit to help prevent, treat and manage disease.”
Chronic diseases that affect African Americans at a higher rate include cancer, diabetes and heart disease. Ewing explains that although genetics alone does not tell the entire story, it can be a very important clue that “opens the door to a new chapter of more precise, safe, and efficient care management, not only for an individual but also for a family.”
“I talk to my girls about our family history of cancer and heart diseases,” Dedmon says. “I normalize the conversation at a very young age so that when they become young adults, they are educated, equipped and empowered to make their decisions about genetic testing and managing their health.”
Here are practical steps one can take to determine genetic makeup:
- Research family health history to include relatives’ diseases, conditions, diagnoses and for those who have died, their age and cause of death. Include both sides of the family —parents, children, siblings, grandparents, aunts, uncles, nieces and nephews. The CDC recommends using the My Family Health Portrait tool to collect information.
- Spread the word. Share family health history with family members and alert your primary physician.
- Schedule an appointment with a genetic counselor, then schedule a medical genetic test. Genetic testing can be done on samples of blood or saliva, or from a swab of the inside of a cheek. The samples are sent to a lab for testing.
- Upon receiving results, share key information with family and doctors.

Dedmon, now 36, educates audiences nationwide about breast cancer prevention and genetic testing in partnership with organizations such as Penn Medicine’s Basser Center for BRCA Black and BRCA Initiative, The Tigerlily Foundation, FORCE and The WISDOM Study to stress the importance of knowing one’s genetic status.
It’s especially important to her to educate younger generations.
“I’m a believer, and the Bible says faith without works is dead, so I needed to get to work, ask questions and protect my health,” she says. “I am confident I made the best health decision for me, my girls and my future.”
Lyndsay Levingston is a multimedia maven, breast cancer survivor and founder of SurviveHER, a breast cancer awareness nonprofit organization whose mission is to inform, inspire and empower year-round.