Polio, short for Poliomyelitis, is a disabling and life-threatening disease that can infect a person’s spinal cord, causing paralysis. Artifacts suggest the disease has existed since ancient times.
An Egyptian stele from 1850-1350 BC depicts a priest lacking muscular strength in his leg. historians believe the stele confirms the existence of the disease thousands of years before there was a name for it. By the 18th century, prominent scientists in Great Britain and Germany developed a clinical understanding of polio. Shortly thereafter, outbreaks were occurring in the U.S., with the most widespread pandemic taking place in the 1940s and 1950s.
Polio is highly contagious, meaning a person can spread the virus even if they aren’t experiencing symptoms. During each year of the 1940s’ pandemic, an average of 35,000 people became disabled. Therefore, parents and guardians were extremely cautious of their child’s whereabouts into the 1950s, when a vaccine was developed.
“When I was a child in the 50s, we had to avoid the swimming pool and had to be in groups of no more than three throughout the whole summer,” Dr. William Haseltine, author of My Lifelong Fight Against Disease: From Polio and AIDS to COVID-19, says to ESSENCE.
How polio affects the body
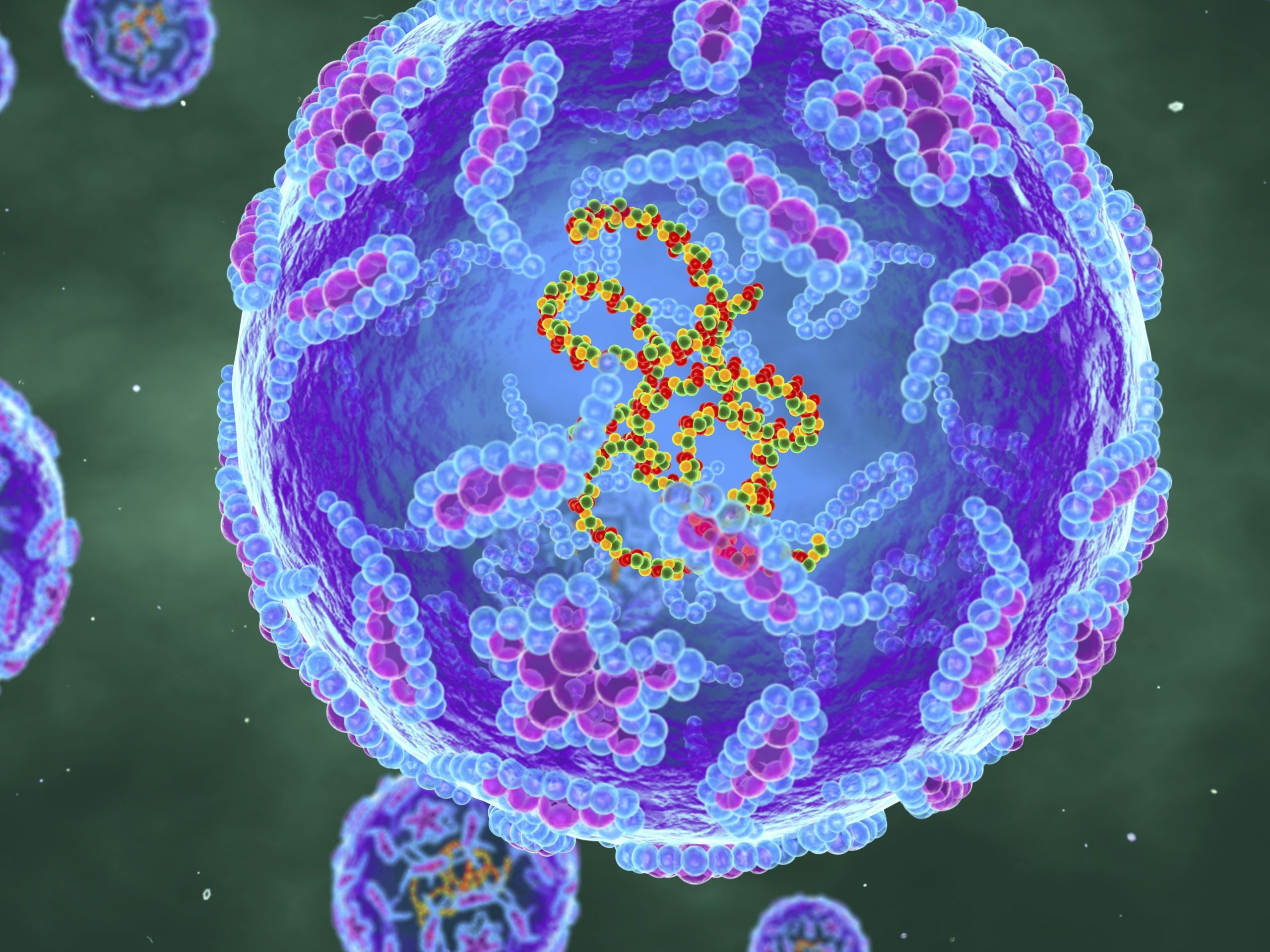
Polio is aggressive and enters the body through the gut. “The virus enters the cells of the gastrointestinal [stomach and intestines] tract by binding to specific proteins called receptors,” explains Dr. Manoj Gandhi, Senior Medical Director at Thermo Fisher Scientific. “Once inside the cells, the viral genetic material is released and the virus uses the host cell’s machinery to help it replicate and make more copies of itself called virions. As these virions are released from the cell, the host cell is destroyed, and the virions go on to infect more cells.”
One of the most well known cases of polio is former U.S. president Franklin D. Roosevelt. After a sailing trip during a 1921 vacation, he complained of lower back pain and his legs became weaker. On the third day after the boat ride, he could no longer hold his weight. He was later diagnosed with polio and used a wheelchair for the rest of his life.
Where he contracted the virus is not confirmed, but they believed it was at a Boy Scout Camp that he attended just before heading to the Island. Normally after a week of contracting polio, paralytic symptoms occur. The virus spread quickly and aggressively, and in his case, crippling him.
“These virions then enter the blood and can spread to the rest of the body. In a small proportion of cases the virus can cross the bloodstream into the Central Nervous System (CNS). How, specifically, the virus is able to get into the CNS is not well understood; but once it affects the CNS, it can destroy nerves that control the muscles and movement. This is known as Acute Flaccid Paralysis, and this damage can be permanent. In very rare cases, when the muscles that control breathing are affected, it can cause respiratory arrest and is fatal.”
The odds of paralysis and death are low, with one in 200 infections leads to irreversible paralysis. Among those paralysed, 5–10 percent of die when their breathing muscles become immobilized.
Polio spreads through transmission. “The polio virus is spread through contaminated hand-to-mouth transmission or putting objects in the mouth that may be contaminated by the virus,” Dr. Gandhi says. As shared, it is extremely contagious so transmission is all too easy.
Polio throughout history
To slow the spread of polio in the 1950s, towns practiced protocols similar to the ones enforced during the earliest days of the Covid-19 outbreak. Churches, schools and theaters were among the places shut down. When Dr. Jonas Salk developed the injectable Polio vaccine in 1955, (followed by Dr. Albert Sabin development of a more effective oral vaccine in 1961), global vaccination campaigns began.
“The sabin vaccine was used very very widely across the world as part of the major efforts to control and eliminate polio,” Dr. Haseltine elaborated.
By 1979, U.S. cases of polio caused by wild poliovirus had ceased. If someone in the U.S. contracted the virus, it was carried through an international traveler. Prior to 2022, the last time the wild poliovirus was brought into the country was 1993.
How polio came back
In July 2022, a case of polio was detected in Rockland County, New York. A 20-year old resident contracted the virus after traveling to Hungary and Poland. Upon his arrival in the states, he was hospitalized and initially diagnosed with Acute Flaccid Myelitis. After more thorough testing, the doctors confirmed that he contracted a strain of polio found outside of the United States.
The individual from Rockland County was not vaccinated, which contributed to his paralysis. Vaccinations were already low in his county to begin with: Rockland and Orange county polio vaccination rates are at 60 percent, compared to 93 percent nationwide by age 2.
“There’s been a major anti-vax movement… As a result of that, a very large fraction of some populations have not been vaccinated for the past 30-40 years against polio…In some parts of the U.S., particularly, rural parts of the U.S. and not heavily urbanized populations, the vaccination rates can be around 50 percent. That means they are subject to infection and paralysis by polio,” Dr. Haseltine details.
The good news is that 92.6 percent of the U.S. population is vaccinated against polio within 24 months of birth. If most of the population remains vaccinated, the number of infections will seize just as in the 70s. In New York, Dr. Haseltine says the current outbreak’s severity is “about a 3 or 4” out of 10.
As shared, polio is highly contagious; but it’s often asymptomatic. For every 200 individuals infected, one becomes paralyzed. Since the case of the individual from Rockland County led to paralysis, the fear is that many in his county and beyond are infected and unaware.
Citizen’s fears are now backed by facts. On August 12, The New York State Department of Health and the New York City Department of Health and Mental Hygiene released a statement saying strains of polio were detected in New York City, Rockland, and Orange County sewers. This means the bodily waste of residents in these counties contained strains of the virus.
“Detecting the virus in the wastewater means that the virus is circulating in the community,” explains Dr. Gandhi. It is also helpful to note that while the virus is not spread through the wastewater; the wastewater confirms that it is spreading. Therefore, the virus is escalating without officials being able to track how to isolate it.
How to protect yourself
There is no cure for polio. The only preventative measure is vaccination.
“There are two types of vaccines. One is the Inactivated Poliovirus Vaccine (IPV) which is given as an injection; second is the Oral Polio Vaccine (OPV), that is given orally using a live attenuated virus,” Dr. Gandhi says. Both these vaccines are effective in preventing Polio. The IPV is the only one that is used in the US, while the OPV is widely used in the rest of the world.”
Attenuated vaccines contain weakened forms of the germ that cause it. Inactivated versions of vaccines contain the killed version of the germ that causes the disease.
***
Dr. Gandhi advises on who should be vaccinated and how many doses they should receive. “The CDC recommends that children get four doses of IPV: 2 months, 4 months, 6-18 months, 4-6 years of age. Most adults should be vaccinated against Polio, but if there are any adults who are unvaccinated or have incomplete polio vaccination, they should get the vaccine.”
If adults have not been vaccinated, the CDC recommends receiving the vaccine in three doses. If individuals are at high risk for polio exposure, one lifetime booster shot is available.
It is not known how long people are protected from polio after receiving the vaccine but the CDC suggests it is years after a completed series. Meaning, an individual received all recommended doses of the vaccine.
All in all, polio is preventable, and we can eradicate it again as a population.