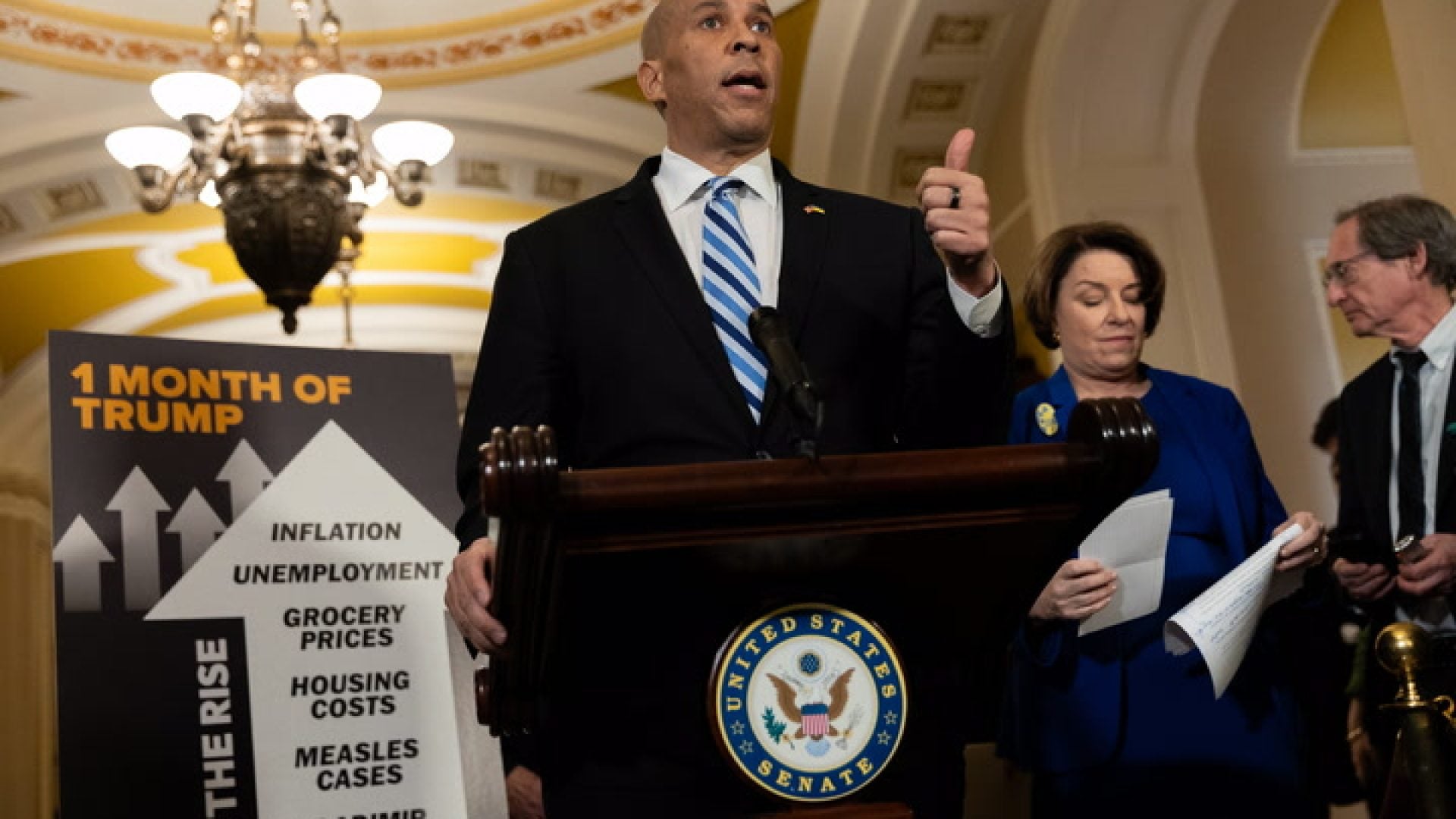
The news of Secretary of Defense Lloyd Austin’s “secret” hospital stay in January 2024 created waves in the political community. Pundits debated the protocol of a senior national security officer being out of commission without the president or the public knowing, but another factor was at play. Secretary Austin received a prostate cancer diagnosis. “The news shook me, and I know that it shakes so many others, especially in the Black community,” he said of his diagnosis. “It was a gut punch.”
One in six Black men will develop prostate cancer during their lifetime, compared to one in eight white men. Black men are 60% more likely to develop it than white men and are 2.14 times more likely to die from the condition than white men. Black men are also more likely to die from low-grade prostate cancer than other races. These rates apply to African American men and men of Caribbean descent. Prostate cancer in Black men may have biological characteristics associated with more aggressive disease. Research suggests that due to inherited genetic factors, differences in tumor biology cause this cancer in Black men to progress faster and/or be harder to treat. So what are Black men doing to prevent such a diagnosis? In many cases, not enough.
Stigmas Around Screenings
Marlon McKnight, a 44-year-old man living in Orlando, has never had a prostate screening and is not looking forward to getting one done. McKnight’s primary care provider has told him he needs to schedule one at some point but hasn’t actually referred him for the test. Speaking of seeking his healthcare provider, McKnight recalls growing up in Jamaica, where “We go to the doctor when we’re sick.” He’s not in a rush, and McKnight says that he is also sensitive about his rectum and doesn’t want anyone touching him there, regardless of the circumstance. “Just the thought of a man behind there with his fingers in me makes me nervous,” he admits.
“Black men in particular, they’re afraid of getting the exam done,” says Brian K. McNeil, MD, MBA, FACS, vice chair of the Department of Urology, The University Hospital of Brooklyn. “There’s a lot of fear out there. A fear of the unknown, and there’s a fear of the consequences of the test.” McNeil says that Black men fear getting bad results. Questions swirl in their minds like, what if I need some sort of surgery or radiation? Am I going to have trouble urinating? Am I going to have to wear some sort of pad or a diaper for a long time?
“Prostate cancer and prostate health, in general, is unique because it could be tied to one’s masculinity,” explains McNeil. He says that some may tie it to their sense of being a man, their virility, and sexual function. “Anything that could have an impact on that or impede that in any way becomes a bit scary,” he adds.
Professor David B. Miller, Ph.D., M.S.W., M.P.H., Case Western Reserve University, says his research shows it’s an intersection of possible homophobia, identity, and mistrust. “So those three factors are at play,” he says. “This doctor is going to put a finger up my butt. Why is he doing this? Something is wrong with them. Are they doing this to me for something else?” Miller says all of that mythology and the conspiracies get mixed up, and then all of a sudden, there’s no longer a desire to be screened or see a doctor.
The Impact of Representation
For Newark, New Jersey’s Jerome Fenton, 40, he has no qualms about prostate screenings. He developed a colon infection at age 30, and his doctor advised that he get his prostate checked at the same time. He intends to do a follow-up screening soon. When asked why he’s so comfortable with the process, Fenton says, “My grandfather passed away from prostate cancer back in like 1990. So my mom has always been big on, ‘You’re not too big or too strong to go to the doctor.’” He shared that his dad has the same kind of attitude. He’s a man who will make an appointment to address his concerns, big or small.
Professor Miller says that when Black men are raised in environments where routine health physicals are normal, there is less fear about seeing the doctor. Conversely, women learn at an early age about gynecological exams. For most men, particularly Black men, prior to a prostate exam, the most invasive testing they experience is a dental exam.
Fenton also thinks that many Black men mostly hear the negative stories surrounding prostate screenings and treatment. While they may hear about someone getting treatment and having to deal with incontinence and erectile dysfunction, they don’t hear and see enough about how medicine and health screenings improve the quality of life.
Distrust of the medical system is also a key factor in the reluctance of Black men to get a prostate screening. Few urologists are actually men of color, so the likelihood of someone being able to see a urologist who looks like them and be able to identify culturally is low.
Keeping Black Men Alive
The first step in getting Black men screened is demystifying the process. What does a prostate screening entail? In the past, it involved the digital rectal examination (DRE). The physician would examine the rectum and feel the prostate for any lumps, bumps, or firmness, coupled with a blood test. “A lot of people have been doing research looking at whether or not the blood test alone is okay,” McNeil says. “Although a lot of organizations still recommend that you get both, some of the latest research is showing that the blood test alone may be enough.”
There are screening recommendations for different ages. Some organizations advise that if you’re between the ages of 55 and 70, you should have a conversation with your doctor about screening for prostate cancer. It is called shared decision-making. You discuss it, and you determine whether or not you want to undergo testing. Most urologic organizations recommend screening between the ages of 50 and 70 years old.
“If you’re part of a high-risk category, maybe you want to have a conversation about screening at the age of 45,” says McNeil, “and if you’re very, very high risk, you might want to consider having that conversation at the age of 40.”
McNeil says your age determines the level of risk, and if you have any men in your family who have been diagnosed with prostate cancer, like a father, uncle, brother or cousin. “The age of that person when they were diagnosed with prostate cancer matters,” he says. “You want to consider whether or not your relative died secondary to complications from prostate cancer.” You may have a relative who was diagnosed with prostate cancer, and it was a low-grade cancer, and they were treated, recovered and lived a long time. But if you’re someone with a family member who was diagnosed with prostate cancer and died within the same year, that’s a very different situation.
Studies have shown that certain genes that are associated with other gynecological cancers may be associated with men having a higher risk of prostate cancer. Particularly, BRCA one and two are associated with an increased risk of prostate cancer. Getting an understanding of your family’s medical history, both paternal and maternal sides, is vital.
“What I have found out is you have to explain it to Black men, why their risk is higher, and the importance of checking on it. It’s about explaining what that means so that they can make an informed decision,” Miller says.
And if it helps to simplify it, McNeil wants Black men to remember that just as with their car, their body requires maintenance. Consider a urologist a part of that upkeep. Good prostate health ensures they pee better, sleep uninterrupted, and enjoy a satisfying sex life. And yes, it can keep them alive. “It’s not all about the finger,” says McNeil. “It’s about helping you save your life.”